PGS: Important Components Of Chromosome Testing
Published: 12/11/2015
ACFS strongly believes that chromosome testing alone is not the sole reason for our significantly improved success rates. Although, it is overwhelmingly the most important component, without the "best" eggs, an excellent embryo/blastocyst culture system, an excellent freeze-thaw program (vitrification), excellent trophectoderm biopsy techniques using laser and uterine transfer techniques, the team at ACFS does not think that they would get the same results.
-
ACFS strongly believes that every woman is genetically pre-determined to make a certain amount of eggs on each stimulation cycle. Because of age, reproductive function gets hammered, mainly because of chromosome abnormalities, not because ACFS cannot get you good day 5 blastocysts. That is why it is important to be aggressive in COH (controlled ovarian hyperstimulation) to get the most and best number of eggs possible; because only some embryos will make it to blastocysts, then only some will be chromosomally normal.
If not stimulated appropriately/aggressively you may still get a lot of eggs but they may be of poor quality producing "poor" quality embryos that may or may not develop to the blastocyst stage. Even if they develop into a blastocyst (day 5 embryo) they may be "incompetent" and not implant and/or have a higher risk of miscarriage (not related to being chromosomally abnormal). Alternately, if not stimulated appropriately, you will get fewer eggs than you are genetically pre-determined to make; and they may also be of decreased quality, either not fertilizing and/or producing poor quality embryos that do not implant. ACFS believes that understimulation is one of the most important factors in why a woman has an unsuccessful IVF cycle.
There is of course the concern about OHSS or ovarian hyperstimulation syndrome. In its severe form, you can be hospitalized and are "very" sick. OHSS can be avoided by not getting the patient pregnant; in other words, cryopreserve or freeze (vitrification) all the embryos, and later transfer than in a subsequent cycle. Also, by not transferring the embryos the woman can be placed on medications that will significantly abate the symptoms of OHSS. Because of the fear of OHSS, some clinics back off stimulation, or will "coast" the patient or increase the amount of medication if not responding well. ACFS respectfully disagrees with this approach and feels that these cycles should be canceled rather than trying to "rescue" the cycle and re-stimulate in a subsequent cycle.
This thinking may support ACFS speculation that "conservative" stimulation protocols may lead to aneuploidy or chromosome abnormalities. And supports ACFS thinking about not under-stimulating patients and maximizing their genetic potential, whatever it is.
Also, ACFS data shows that pregnancy rates are decreased if you transfer embryos back in a fresh physiologically overstimulated cycle. You may then ask, " then don't physiologically overstimulate me". The problem is if you are not mildly "overstimulated", you may not make the "best" quality eggs/embryos.
- ACFS no longer does day 3 embryo biopsy and a fresh embryo transfer. ACFS published a study in June 2011 showing that 64% of day 3 biopsied embryos that make "nice" looking blastocysts but that come back chromosomally abnormal, if re-biopsied on day 5, "self-correct" and are chromosomally normal. Also, it has been shown that embryos like group culture and if biopsied on day 3 have to be separated and kept in their culture dishes to keep track. It would also mean a fresh transfer in a potentially physiologically "overstimulated" cycle. And since only the "best of the best" embryos make it to day 5; if embryos do not make it to the blastocyst stage (stage 5) then no biopsy is done and the patient not only knows the answer sooner rather than waiting for the results of the day 3 biopsy; but also saves a considerable amount of money by not doing a transfer. ACFS has not done day 3 transfers in the last 4-5 years with or without chromosome testing.
-
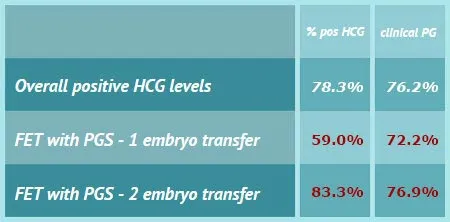
But then you may ask, "is a frozen or cryopreserved cycle as good as a fresh cycle?" In the ACFS experience, a frozen cycle is better than a fresh cycle. Why? For three reasons. First, you do not want to put embryos back in a "physiologically" overstimulated cycle (having adverse effects on endometrial receptivity and endometrial DNA patterns); second, only the "best of the best" embryos survive the freeze-thaw process; and third, it significantly decreases (or can eliminate) the risk of OHSS. This is based on the assumption that your ART laboratory operates at a high level of excellence. ACFS was not able to say this 5-6 years ago, but if your embryos were not able to reach the blastocyst stage (day 5) in the ACFS-ART laboratory culture system, then they would not have made it in you if they were transferred. The same is true of frozen embryos, if they do not survive the freeze/thaw process (vitrification) at ACFS then they would not have survived in a fresh transfer. Some clinics disagree with these conclusions but the overall experience at ACFS is quite the opposite. Recent reports in the literature (ESHRE, July 2012) support ACFS conclusions. Initial meta-analysis on this subject indicates that the chance of a clinical pregnancy is approximately 30% higher when all the embryos are frozen or cryopreserved (vitrification) for later transfer than with fresh embryo transfer. We have not done a day 3-embryo transfer for the last 4-5 years; and as shown from our data above, we feel very comfortable with our freeze/thaw (or vitrification) program which is a very critical part of doing PGS-chromosome testing.
This also works out quite well because if you are doing chromosome testing, the embryos are cultured out to day 5 or the blastocyst stage, than biopsied. Since you do not get the results in time to do a fresh transfer, all the embryos are cryopreserved and transferred in a subsequent cycle (FET-frozen embryo transfer); thus avoiding transferring them back in a "physiologically" overstimulated cycle and also avoiding the risk of OHSS. Two very important advantages.
- ACFS knows what it is asking, that women not do a fresh transfer and wait to do a FET or frozen embryo transfer. The goal however, "is not to see how fast we can do the procedure" but to maximize the chances of getting pregnant on the first attempt at IVF. ACFS' data supports this premise. Even if a couple is not doing chromosome testing, they should consider not doing a fresh transfer in a physiologically overstimulated cycle, cryopreserve all their embryos and subsequently do a frozen embryo transfer (FET) the following cycle. Most folks then say, "but data shows that fresh is better than frozen". Actually, in ACFS experience this is not accurate. Why? Because in a regular IVF cycle without chromosome testing, the "best" looking embryos (morphologically normal) are transferred in that fresh cycle and the "remaining" embryos are then cryopreserved. Statistically, however, "these remaining embryos" tend not to be the "best embryos" (hence, why they were frozen instead of transferred). Subsequently, when doing a future FET with these "lesser quality" embryos, pregnancy rates are not as good. In contrast, if ALL the embryos had been frozen, and only the ones that survived the freeze-thaw process were transferred, pregnancy rates would be as good, if not higher, than a fresh transfer.
- The "easy" job at ACFS is to get good day 5 blastocysts, even in reproductively older women. ACFS is very good at that and can control the whole thing-from ovarian stimulation (COH), fertilization using ICSI, blastocyst culture developing the embryos to day 5, the freeze-thaw process (vitrification) and uterine transfer. Where we "lose" control is whether or not the embryos are chromosomally normal. That is out of ACFS's control. Therefore, it is ACFS thinking, "If you can not control it then maximize it".
- A very important component of chromosome testing (PGS) is the skill and expertise of the embryologist doing the biopsy. There are only a limited number of embryologists that had the expertise and experience to safely and effectively do day 5 blastocyst biopsies with laser. ACFS embryologist has done over 1500 blastocyst biopsies without harming a single embryo. This is not the kind of procedure that you would want to be done by someone that does not do it regularly.
- ACFS also recommends that reproductively older women, in addition to doing chromosome testing, also consider doing two stimulation cycles. The first cycle would be to only get eggs which would be cryopreserved (vitrification) and then let the patient get her period. In one or two months, she would stimulate again. Then, the eggs from the first stimulation cycle would be thawed and along with the fresh eggs from the second stimulation cycle, all be fertilized; only paying one ICSI charge, one advance culture (blastocyst) charge, one TE biopsy and chromosome charge. The advantage of doing this is that as women get reproductively older they make fewer eggs/embryos that advance to day 5 blastocysts and that are chromosomally normal. By doing two stimulation cycles, you get twice as many eggs/embryos that have a chance to reach the blastocyst stage and be chromosomally normal; thus increasing pregnancy rates and decreasing costs. This all depends on the ART-IVF lab having an excellent egg vitrification or vitrification program. ACFS data shows that egg vitrification or freezing is as good as using fresh eggs.
- ACFS does not transfer using ultrasound guidance and has data showing that it is not necessary. By not using ultrasound-guided uterine embryo transfer, it is much more comfortable for the patient by not having 32-40 oz. of water in the bladder and having a large speculum in the vagina while someone is pushing down abdominally on your bladder. ACFS did an internal study approximately 8 years ago and showed the uterine embryo transfer (ET) with a mock transfer first was more successful than ultrasound-guided ET.
- ACFS does not do this for money. We do chromosome testing (PGS) at our cost because we want all patients to consider doing PGS with their IVF cycle. Hopefully, by a patient getting pregnant on their first attempt, ACFS loses money by not doing multiple attempts at either a fresh and/or multiple FETs (frozen embryo transfer). If there are no remaining chromosomally normal embryos, ACFS losses it's freezing fees and storage fees.
- Is ACFS biased with its IVF success rates? We are. But it is biased solely in favor of the patient. We do not think that any woman would knowingly want to transfer chromosomally abnormal embryos. By knowing that you have chromosome normal day 5 blastocysts that survived the freeze-thaw process, ACFS is biasing the results. But that's a good thing.
WHAT DO YOU THINK WILL HAPPEN IF YOU TRANSFER TWO NICE-LOOKING DAY 5 BLASTOCYSTS THAT ARE CHROMOSOMALLY COMPETENT AND HAVE SURVIVED THE FREEZE-THAW PROCESS WITH AN UNEVENTFUL UTERINE TRANSFER?