In Vitro Fertilization (IVF) in Phoenix, AZ
What is IVF?

In vitro fertilization (IVF) is a procedure in which eggs collected from a woman’s ovaries are combined with sperm in an embryology laboratory to enable fertilization of the eggs and the development of one or more embryos, which can be transferred to the uterus to establish a pregnancy.
Usually, a single round of ovarian stimulation and egg retrieval is referred to as an “IVF cycle.” It takes approximately 2 weeks to stimulate the ovaries and retrieve eggs. The embryo transfer may be performed in the same cycle (3-5 days after egg retrieval, i.e. “fresh IVF”) or in a later frozen embryo transfer (FET) cycle.
Arizona Center for Fertility Studies IVF Process
The key elements of the IVF treatment process are as follows:
-
Pre-IVF Start Visit: Before it all begins, we will schedule you for an appointment where you will have a baseline ultrasound to check for ovarian cysts. At this visit, we will review your personalized IVF calendar, instruct you on when and how to take your medications and ensure that all of your questions about the IVF treatment process have been answered.

-
Ovarian stimulation: You will take fertility medications for approximately 10-12 days to help grow and develop as many eggs as possible while also taking medication to prevent premature ovulation. Eggs are contained within ovarian follicles. The primary medication driving follicular development, not surprisingly, is called follicle-stimulating hormone (FSH), a hormone that is naturally produced by the pituitary gland. FSH and the other key fertility medications are typically given by subcutaneous injection, which most patients find easy to do themselves after some initial coaching.

-
Follicular Monitoring: We monitor response to stimulation and ovarian follicle development with frequent ultrasound visits and hormonal assessments. During these 4-5 visits, the follicles and uterine lining are measured, and medication dose adjustments may be recommended.

-
Trigger: Final maturation of the eggs is “triggered” with an injection of hCG and/or Lupron (leuprolide) when it is anticipated that a majority of the eggs are ready, based upon follicle sizes and hormone levels. We are typically looking for a minimum of 2-3 follicles measuring 17-18 mm or greater in average diameter and are hoping to recover a single egg from each follicle greater than 14 mm. The trigger is usually administered 34-37 hours before egg retrieval.

-
Egg retrieval: The eggs are recovered by ultrasound-guided transvaginal aspiration of the follicles under IV sedation. You will be asleep and comfortable but breathing on your own with this type of sedation. As the procedure is taking place, the fluid aspirates obtained from the ovaries are given to the embryologist in the adjacent IVF laboratory through a pass-through window. The embryologist will isolate each cumulus-oocyte complex and determine the number of eggs obtained and their maturity. This procedure takes approximately 30 minutes and is followed by an additional 30-45 minutes of recovery time at the fertility center. When you are ready to go home, you will need a designated driver and should plan to take it easy for the rest of the day. You should be able to return to non-physical work and most normal day-to-day activities the following day.
-
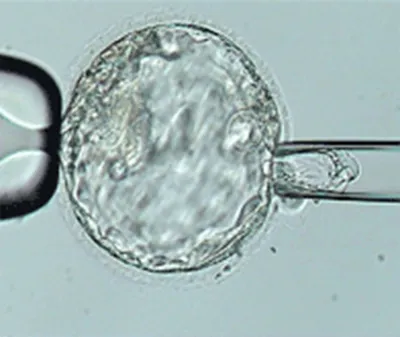
Fertilization: Once the eggs are in the lab, each egg is combined with thousands of sperm within a small droplet of fluid in a petri dish for conventional in vitro fertilization, or a single sperm is introduced into each mature egg by intracytoplasmic sperm injection (ICSI). The next day the eggs are evaluated under a microscope to confirm that normal fertilization occurred. Typical fertilization rates are greater than 50-70% for conventional IVF and greater than 90% for ICSI.
-
Embryo culture: The newly-fertilized eggs, or embryos, are grown in the lab for 5-6 days in most cases. Embryos should typically contain 2-4 cells by day two, 6-10 cells by day three, and hundreds of cells by day five of development. At ACFS, we prefer to freeze and transfer embryos that have proven their ability to develop to the day 5-6 blastocyst stage rather than to transfer them just 2-3 days after fertilization. We expect roughly 60% of normally-fertilized eggs to become blastocysts. All of your embryos will be graded before cryopreservation, and we will use the grading to help decide which of your healthy embryos will be given priority for transfer.
-
Trophectoderm biopsy: This step is necessary when using preimplantation genetic testing (PGT) to help select the embryos for transfer. Trophectoderm biopsy removes five to ten cells from the portion of the embryo that forms the placenta, taking care to avoid disturbing the cells of the inner cell mass, which may eventually form the fetal portion of the pregnancy. The trophectoderm cells that are removed are sent to a specialized laboratory for extraction and amplification of their DNA and determination of their genetic status. It takes approximately 1-2 weeks for chromosome testing results to come back. The embryos remain safely stored at ACFS while waiting for these results.
-
Embryo cryopreservation: Embryos that are undergoing PGT or future FET are cryopreserved at ACFS using the latest vitrification techniques. Freezing the embryos provides time to obtain chromosome testing results and allows hormone levels to return to normal before attempting embryo transfer, resulting in the highest possible pregnancy rates.

-
Embryo transfer: In fresh IVF, the embryos are transferred into the uterine cavity 2-6 days after egg retrieval. In frozen embryo transfer cycles, the transfer happens in a separate cycle in which the uterus is prepared with estrogen and progesterone. The transfer is carefully timed to the first rise of progesterone because this is how the embryo is synchronized to the uterus for successful implantation. This procedure is not painful and does not require anesthesia or extended bed rest. You will be able to see your embryo before the embryo transfer procedure and can watch the procedure take place under ultrasound guidance.

-
Pregnancy test: We will schedule your first blood pregnancy test (beta-hCG) as early as 9-10 days after embryo transfer, which corresponds to approximately “4 weeks” gestational age. Sometimes we will recommend repeating the test to ensure that the hCG levels are rising normally. Very fortunately, this test is positive for over 80% of our patients using IVF with PGT and frozen embryo transfer. A large majority of patients with a positive pregnancy test after IVF with PGT and FET will go on to deliver a baby.

-
First ultrasound: This is the moment we’ve all be waiting for! We will schedule your first ultrasound at approximately “6 weeks” gestation, which is about 2 weeks after the first positive pregnancy test. At this time, we will usually see the early pregnancy and the flicker of a fetal heartbeat, which is amazing considering how early and small the pregnancy is at this stage!

-
Early pregnancy monitoring: We follow our patients forward until they have fully transitioned to their obstetrician’s care, usually at the end of the first trimester. Many of the support medications for IVF must be continued after embryo transfer, so we will advise when it is safe to stop medications and when others should be continued. The last ultrasound visit at ACFS is usually filled with mixed emotions. We are thrilled when our patients surpass this major milestone in their fertility journey, but we have a hard time letting you go! We love it when patients keep in touch with us throughout their pregnancy and plan a visit with us at ACFS after delivery so that we can meet all of the #babiesbyshane after they’re born.

Request Your Consultation Today!
If you want to learn more about in-vitro fertilization (IVF), call your ACFS fertility team today at (480) 860-4792.











