Solutions For Multiple Unsuccessful In-Vitro Fertilization (IVF) Cycles
Published: 12/14/2015
Unfortunately, not all patients are successful even after doing multiple attempts at In-Vitro Fertilization (IVF). This can be due to a number of reasons including maternal age, elevated FSH levels, poor responses to fertility medication, decreased number of eggs aspirated, decreased rates of fertilization, decreased numbers of embryos available for transfer, decreased quality of embryos, unexplained factors, and variation in the experience and expertise of the embryology laboratory. Thus, couples presenting with repeated implantation failure (RIF) represent a significant challenge for the treating clinic.
There are a number of options for multiple unsuccessful cycles of In-Vitro Fertilization (IVF):
- Make sure that the entire work-up has been done, including testing (things can change) that is more than one year old and "controversial tests" like antisperm antobodies (ASA) and antiphospholipid antibodies (APA). You need to have a hysterosalpingogram to document that your tubes are open. Closed tubes, or hydrosalpinges, can fill with fluid that can backflow into the uterus and be toxic to implantation. Also, a recent sonohysterogram. Water is injected into the uterine cavity which is viewed with transvaginal ultrasound for filling defects. It is needed to rule out any uterine pathology like polyps or fibroids. At Arizona Center for Fertility Studies, our policy is to have a SHG within three months of a uterine transfer. We have seen a normal cavity change in as little as 4-5 months. If APA and/or ASA testing is positive, either one can interfere with pregnancy outcome. Positive APA may interfere with the very early blood flow to the uterus and interfere with implantation. A positive ASA may cause antibodies to attack the paternal contribution of the pregnancy and cause a very early miscarriage, before a woman even knows she is pregnant.
- Make sure that you are maximally stimulated for your age. All clinics are concerned with overstimulation and the risk of ovarian hyperstimulation syndrome (OHSS). This is a process in which the ovaries can become enlarged and allow large amounts of fluid to pass across them into the abdomen sometimes resulting in a very sick patient that needs hospitalization. Although OHSS needs to be taken seriously, it has been the experience at Arizona Center for Fertility Studies, that not giving enough medication for a woman's age or circumstances; or cutting down on the dosage of medication, may reduce the risk of OHSS, but it may also cut down on the amount of hormones needed to adequately stimulate normal follicular (egg) production resulting in decreased numbers of eggs, decreased quality of eggs and resulting embryos, and decreased pregnancy rates. Giving less fertility medication doesn't necessarily produce less eggs, it may produce the same number of eggs, but with each egg getting less hormonal stimulation to their receptors and resulting in poor egg quality.
- Not all clinics are created equally, and more specifically, some embryology laboratories have more experience and expertise than others. This could definitely result in different outcomes in pregnancy rates and ongoing pregnancies. Although looking at a clinic's success rates are important, you are not always comparing "apples to apples" (In-Vitro Fertilization (IVF)). Some programs are better than others and consistently get better success rates, even with more difficult patients. The reasons are sometimes difficult to ascertain and explain why. At Arizona Center for Fertility Studies, the more things we can do differently than what you have already done, the greater the odds are that we can be successful. If we did things the same way as what you have already experienced in the cycles that were unsuccessful, then we would expect the same result. That does not mean that the clinic you were at did not do things "right". On the contrary, it just means that there are different philosophies on how to do things based on experience. Sometimes, to be successful, it takes an additional attempt at a clinic that consistently has high success rates. That clinic, however, needs to be forthright, to let you know, after carefully looking at your entire medical history and embryology laboratory work sheets, if they honestly feel that you can be successful at their program.
- After all factors have been considered and you have exhausted all the other options with In-Vitro Fertilization (IVF), and you have still have not been successful, then you need to consider doing something else. Although donor eggs is always an option, there is another and possibly very successful option to consider - ZIFT or zygote intra-fallopian tube transfer or GIFT (gamete intrafallopian tube transfer). ZIFT is a procedure where your eggs are recovered and fertilized exactly the same as with In-Vitro Fertilization (IVF), but rather than keeping them in the incubator, they are immediately transferred back into the fallopian tube via laparoscopy within a day or two. GIFT is a procedure where the eggs are recovered by either transvaginal aspiration or laparoscopy, immediately mixed with sperm and placed back into the fallopian tube, all within a matter of minutes. With GIFT, it allows procreation to occur in the body, which for some religious beliefs, is the only "allowable" means of advanced reproductive technology. Although, the Roman Catholic Church is against all advanced reproductive technologies, including GIFT, but especially ZIFT and In-Vitro Fertilization (IVF); the American Catholic Church approves of the GIFT procedure, but not ZIFT and In-Vitro Fertilization (IVF). The reason to consider the option of either GIFT or ZIFT is the thinking that some embryos do better in the "natural environment" of the fallopian tube rather than the "artificial environment" of the incubator. It could also allow further and more advanced development in the natural environment of the fallopian tube before entry into the uterine cavity, greater synchronization with the uterus, the presence of numerous growth factors in the human tubal fluid may contribute to the development of some early embryos and thus enhance implantation, and may do away with a traumatic cervical transfer in some difficult patients. The problem, of course, is how to identify these embryos in advance. It has been demonstrated in numerous scientific articles that pregnancy rates do not significantly change over the first three attempts at In-Vitro Fertilization (IVF), but decrease by 40% or have less than 5% chance of success after four or more prior failed attempts. Said differently, there is a high and similarly equal chance of success on the first three attempts at In-Vitro Fertilization (IVF) but if not successful, then a fourth attempt will offer little success unless there has been a major change in protocol, like the possibilities mentioned in paragraphs 1, 2 and 3, or the "environment" that the embryos are placed into is changed. Depending on a number of different studies, success rates with ZIFT, after three or more unsuccessful attempts at In-Vitro Fertilization (IVF) approaches 40%, depending on the patient's age and circumstances. Arizona Center for Fertility Studies has probably more experience with GIFT and ZIFT than any other clinic in the world and is one of the few clinics in the United States that offers GIFT and ZIFT as an alternative to having to go with donor eggs.
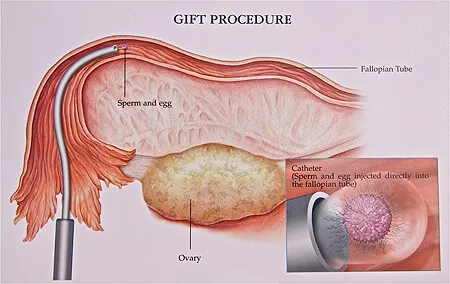
GIFT or gamete intra-fallopian tube transfer - where sperm and eggs are mixed immediately after egg recovery and injected directly into the fallopian tube, allowing fertilization to occur in the fallopian tube
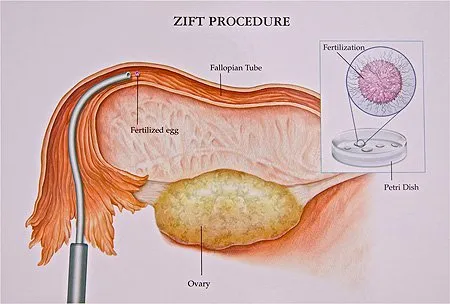
ZIFT or zygote intra-fallopian tube transfer - a procedure where the eggs are fertilized outside the body and as soon as fertilization is visibly documented the less than 24 hour old embryos are transferred into the fallopian tube
- A number of different treatment modalities have been recommended and attempted for unsuccessful In-Vitro Fertilization (IVF) to better improve implantation in these patients. These treatments include the options of assisted hatching where a microscopic hole is made in the wall of the embryo to help it "hatch out" before implantation, embryo co-culture, PGD/PGS pre-implantation genetic diagnosis where a single cell is removed from a day 3 embryo and sent for chromosome analysis (Preimplantation Genetic Diagnosis - PGD/PGS ), prophylactic removal of the fallopian tubes in the cases of large hydrosalpinges or dilated water tubes, and even extended culture to day 5 or blastocyst stage (Blastocyst Transfer). Unfortunately, all these factors should have been considered on the first attempt at In-Vitro Fertilization (IVF), not the third.
- At Arizona Center for Fertility Studies, we have found one additional option that has proven successful in patients with repeated unsuccessful attempts at In-Vitro Fertilization (IVF) - that is the addition of human growth hormone or hGH to the treatment protocol. It is a known fact that hGH is a co-gonadotrophin and, like FSH and LH, is absolutely needed for the full and final maturation of an egg. Although, if measured, a patient will have a normal level of hGH in the blood, some patients do not have enough hGH for all the extra eggs that they make. These patients are impossible to identify "up front" but young patients that make a lot of eggs and have poor fertilization rates or do not get pregnant as expected; or women over the age of 38-39, in Arizona Center for Fertility Studies experience, and backed up by the scientific literature, seem to have better success rates when adding hGH to their treatment protocol. At Arizona Center for Fertility Studies, it is our policy that all women 38 or older are offered the option of using hGH, as part of their starting protocol for In-Vitro Fertilization (IVF).











