Fibroids vs Endometriosis: Impacts on Pregnancy
Published: 12/14/2015
What is Endometriosis?
Endometriosis can be a painful, chronic disease that affects up to 16% of infertile women and occurs when tissue that lines the cavity of the uterus or endometrium is found outside the uterus - most commonly in the abdomen on the ovaries (sometimes forming a cystic cavity full of blood known as an endometrioma), fallopian tubes, uterus, the lining of the pelvis, bladder and the bowel. Endometriosis is generally more common in Caucasian women in their late 20's and 30's. One of the most common theories, as to the cause of endometriosis, is that during normal menstruation, the "menstrum" or menstrual tissue, not only comes out of the vagina as menstrual blood but flows backward through the fallopian tubes and implants on the above-mentioned sites. Once "implanted", these growths or lesions respond each month, hormonally, to the menstrual cycle in the same way that the normal lining of the uterus does. Each month the tissue builds up, breaks down, and sheds. Menstrual blood in the uterus can exit through the vagina but the tissue and blood shed by these "endometrial implants" have no way of leaving the body. This causes internal bleeding and inflammation of the surrounding tissue; resulting in pain, scar tissue and adhesion formation, and possible infertility.
Although, the classic signs of endometriosis are painful periods, pain during intercourse, and infertility; some of the worst endometriosis can be pain-free. Endometriosis is also associated with repeated pregnancy loss, irregular periods and ovulatory dysfunction. On the other hand, the best treatment for endometriosis is pregnancy.
What are Uterine Fibroids?
Uterine fibroids, on the other hand, are benign or non-cancerous growths or tumors, in women of childbearing age, arising from the muscle of the uterus or myometrium. They are made up of connective tissue that grows within the muscular walls of the uterus. They can grow as simple fibroids or in clusters. These benign tumors can be as small as an inch in size or can grow to eight or more inches. No one is sure what causes fibroids to develop or stimulate their growth but fibroids can lay dormant for months, or even years then, all of a sudden, double or triple in size. Current statistics show that they are 3-5 times more common in African-American women; and slightly increased in women that are overweight for their height and decreased in women that have given birth. The biggest stimulus to fibroid growth is pregnancy, and thus, could cause problems with implantation of the embryo, placentation or development of the placenta, first and second-trimester loss, prematurity, premature rupture of the membranes (bag of water), and a breech presentation.
Fibroids can grow on the outer wall of the uterus or subserosal; in the muscle of the uterus or intramural; or right under the lining of the cavity or submucosal, or in the cavity of the uterus, known as intracavitary. The second worst place for fibroids to grow is in the muscle of the uterus (intramural) because they can push into the cavity of the uterus and compromise the blood flow to the baby or push outward and make the uterus think it is bigger than it is and result in premature labor. The worst place for fibroids is in the cavity of the uterus (intracavitary) because that is where the baby grows and results in the biggest risks of complications. Fibroids on the outside of the uterus (subserosal) can generally be a little bigger before they cause problems in having the uterus think that it is bigger than it is and causing premature labor that may or may not be able to be stopped with bed rest, prolonged hospitalization and medications.
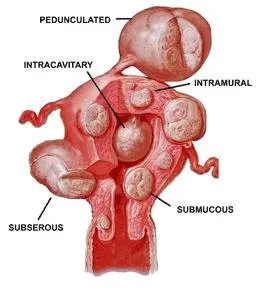
Graphic representation of locations and different types of uterine fibroids
Fibroids, Endometriosis and Pregnancy
Many times, patients are told that their endometriosis or fibroids are not a problem and that they can go on and have a successful pregnancy without complications. Although that can be true in many cases, in others, endometriosis and/or fibroids, can and will prevent you from conceiving or increase your risks of a miscarriage. Patients need to know both possibilities, as well as the risks and complications if nothing is done, and all available options. Many couples do not want to take the risks of not getting pregnant or worse, having a premature delivery, where the baby could have several complications or lifelong problems.
If surgery is recommended, it should be done by someone who has extensive experience and expertise. If a woman is in the childbearing years and has no children or still wants or is thinking about having more children, then a hysterectomy is never an option. Far too often, this is the option women are given by their doctors. Endometriosis can be surgically removed and if there is already too much resulting scar tissue and adhesions from long-standing disease, the latest data in the literature suggests that endometriosis does not affect the outcome of IVF. If there is pain and pregnancy can be postponed, there are very effective medical therapies that will alleviate the pain and "buy time". If there are multiple and/or large fibroids, they can be removed successfully and with minimum to no resulting scar tissue. Although there are other options to shrink fibroids, including the use of lupron and/or uterine artery embolization, both will result in the growth of the fibroids as soon as pregnancy occurs and possibly lead to the above-mentioned complications.
If your doctor has advised you that surgery is necessary and you are planning to have a baby now or in the future, be sure to ask a lot of questions. If the word "hysterectomy" is discussed or even brought up, get out. This includes asking about the way they plan to perform the surgery. How many of these surgeries have they done? What is their complication and success rates? Are they the best qualified to perform this type of surgery? And most importantly, if this particular surgery can affect your future fertility. In my experience, sometimes gynecologic surgeries performed by excellent surgeons can unknowingly result in future difficulties with conception. In many cases, when fertility preservation is important, it may well be worth seeking a second opinion.
Although, there is no way to know if surgery is "needed" or not, a physician's opinion is just that, an opinion. Ultimately, it should be left up to the couple to decide whether or not they want to take the risks. If the doctor has taken care of patients with fibroids that have had a good outcome, they probably will recommend not removing them. If they have taken care of patients who have had a bad outcome secondary to their fibroids, then they are going to recommend surgery to remove them. The problem is, there is no way of knowing for sure. No one can say for sure that the fibroids will result in pregnancy complications; but the one thing that you can say for sure, is that by not removing them, you statistically will increase your risk of having complications. There are times when surgery is done to remove fibroids, that if not done, would have resulted in a good outcome, but the couple should be given that choice. In ACFS experience, most women do not want to take the chance of having a bad outcome, and if given the choice, elect to do the surgery and have no regrets. When you deliver a healthy baby at term, nobody second guesses whether or not they should have done the surgery.











